Regeneration, Repair and Healing
Regeneration
It means the restoration of original structure and function, lost during the inflammation.
Repair
It implies filling up of gap created by the inflammation with non- functional scar tissue.
Healing
It implies the disappearance of the process of inflammation and its replacement by either regeneration or repair or both in varying proportions.
Regeneration and Repair
Regeneration is the renewal of a damaged tissue or a lost appendage that is identical to the original one. Regeneration requires a population of stem or precursor cells with the potential to differentiate and replicated. The regeneration of injured cells and tissues involves cell proliferation which is driven by growth factors and is critically dependent on the integrity of the extracellular matrix.
Several cell types proliferate during tissue repair. These include the remnants of the injured tissue, vascular endothelial cells and fibroblasts. The proliferation of these cell types is driven by proteins called growth factors. The production of polypeptide growth factors and the ability of cells to divide in response to these factors are important determinants of the adequacy of the repair process. Biochemical signals draw the stem cells to sites where growth factors have created an environment for regeneration.
Growth factors
They induce cell proliferation by binding to specific receptors and affecting the expression of genes whose products typically have several functions.
- They promote entry of cell into the cell cycle
- They relieve blocks on cell cycle progression thus promoting replication
- They prevent apoptosis
- Enhance the synthesis of cellular proteins in preparation for mitosis.
- Stimulate the function of growth control genes because mutations in them lead to unrestrained cell proliferation characteristic of cancer.
Below is the list of few common growth factors along with their sources and functions:
| Growth Factors | Sources | Functions |
| Epidermal Growth Factors(EGF) | Activated by macrophages, salivary glands, keratinocytes and many other cells. |
|
| Keratinocyte growth factor (KGF) | Fibroblasts |
|
| Hepatocyte growth factor (HGF) | Fibroblasts, stromal cells in the liver, endothelial cells. |
|
| Vascular endothelial growth factor (VEGF) | Mesenchymal cells |
|
| Platelet derived growth factor (PDGF) | Platelets, macrophages, endothelial cells, smooth muscle cells, keratinocytes. |
|
Role of Extracellular Matrix
Repair of tissue after injury depends on the synthesis of a fibrous extracellular matrix to replace lost or damaged tissue. Newly deposited extracellular matrix is then re-modeled over time to emulate normal tissue. The extracellular matrix directs repair by regulating the behavior of the wide variety of cell types that are mobilized to the damaged area in order to rebuild the tissue. Acute inflammation, re-epithelialization, and contraction all depend on cell-extracellular matrix interactions and contribute to minimize infection and promote rapid wound closure. Matricellular proteins are up-regulated during wound healing where they modulate interactions between cells and the extracellular matrix to exert control over events that are essential for efficient tissue repair
Process of Healing
The healing process is more or less identical in all types of tissue damage, be it inflammatory damage or injuries. The latter situation is covered by the term wound, which simply means damaged tissues generally by physical injury. Healing of wounds is not possible without the participation of inflammatory cells chemical mediators and blood vessels that are also the essential components of an inflammatory process.
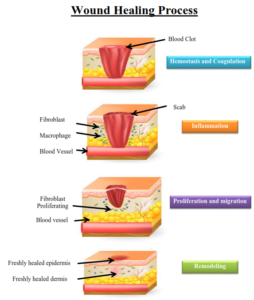
The wound healing process is a dynamic one which can be divided into three phases.
- Inflammatory phase
- Proliferation phase
- Maturation phase
- Inflammatory phase
The inflammatory phase is the body’s natural response to injury.During inflammatory phase 2 major processes take place:
- Clotting
Healing of a wound begins with clot formation to stop bleeding and to reduce infection by bacteria, viruses and fungi. Clotting is followed by neutrophil invasion three to 24 hours after the wound has been incurred, with mitoses beginning in epithelial cells after 24 to 48 hours .
- Inflammation
In the inflammatory phase, macrophages and other phagocytic cells kill bacteria, debride damaged tissue and release chemical factors such as growth hormones that encourage fibroblasts, epithelial cells and endothelial cells which make new capillaries to migrate to the area and divide.
2. Proliferation phase
During proliferation, the wound is ‘rebuilt’ with new granulation tissue which is comprised of collagen and extracellular matrix and into which a new network of blood vessels develop, a process known as ‘angiogenesis’. Healthy granulation tissue is dependent upon the fibroblast receiving sufficient levels of oxygen and nutrients supplied by the blood vessels. Healthy granulation tissue is granular and uneven in texture; it does not bleed easily and is pink / red in colour. The colour and condition of the granulation tissue is often an indicator of how the wound is healing. Dark granulation tissue can be indicative of poor perfusion, ischemia and / or infection. Epithelial cells finally resurface the wound, a process known as ‘epithelialization’. 3.Maturation phase
Maturation is the final phase and occurs once the wound has closed. This phase involves remodeling of collagen from type III to type I. Cellular activity reduces and the number of blood vessels in the wounded area regress and decrease.